Your prostate is a gland below your bladder, in front of your rectum. Connective tissues and glandular tissues make it up. It adds fluids to your semen. Its muscles also help push semen through your urethra and out of your body. It naturally gets bigger as you get older. But other conditions that affect it include prostatitis and cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
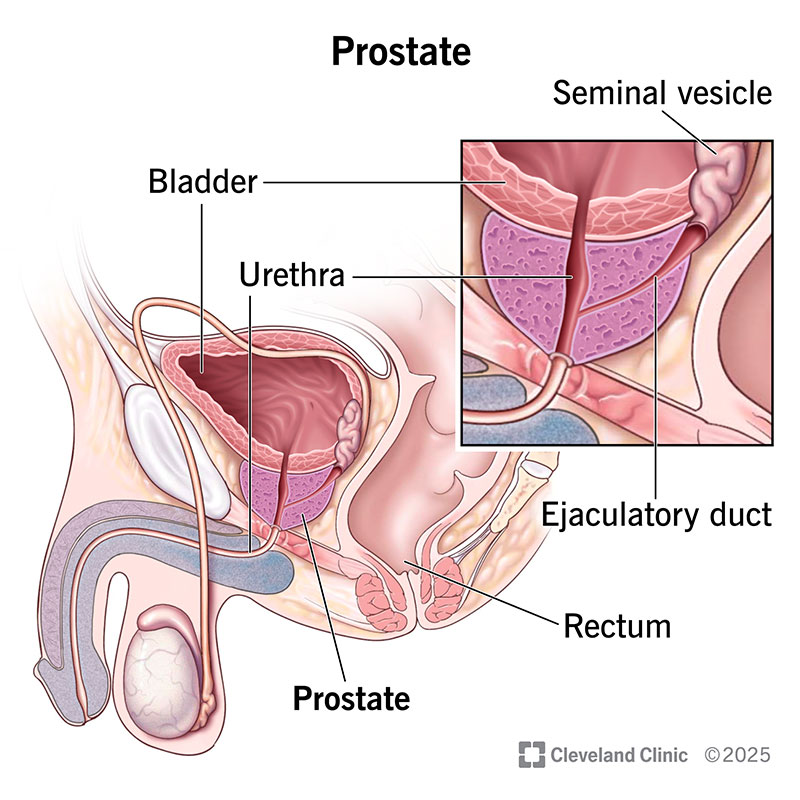
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/prostate)
The prostate is a small, firm, partly muscular gland that helps make up the male reproductive system. It surrounds part of your urethra. It creates fluids that help make up semen. Semen is the fluid that carries sperm during ejaculation. It leaves your body through your urethra, usually after an orgasm.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your prostate gland makes extra fluid in your semen. The fluid contains enzymes, zinc and citric acid. These components help nourish sperm cells and lubricate your urethra. Muscles in your prostate also help push semen into and through your urethra when you orgasm.
No, females don’t have prostates. But they have Skene’s glands. Experts believe they release fluid that helps with peeing, cleanliness and lubrication during sex. They may also release fluid during orgasm, like males. Some people refer to Skene’s glands as the female prostate.
Your prostate is below your urinary bladder and in front of your rectum.
Your prostate is about the size of a walnut. It weighs about 1 ounce (30 grams), which is as heavy as five U.S. quarters. As you age, your prostate usually gets larger. It can grow to the size of a lemon.
Your prostate has five lobes, or sections:
Connective tissues and glandular tissues make up its structure. Prostatic fascia covers your prostate. Prostatic fascia is like a hot dog casing. It’s a sheet of thin, stretchy connective tissue that holds your prostate in place.
Common conditions that can affect your prostate include:
Advertisement
It depends on the cause. But in general, prostate conditions usually cause conditions like:
Your healthcare provider can check the health of your prostate with:
You can help keep your prostate healthy by:
Advertisement
Dietary supplements don’t have to go through clinical trials or get approval from the United States Food and Drug Administration (FDA). So, there isn’t a lot of data on them. They may show minor benefits. But most people won’t see their prostate health improve if they take them.
Yes. Sometimes, healthcare providers recommend removing your prostate to treat prostate cancer. You can live without a prostate. But it may cause changes in your day-to-day life. Common prostatectomy side effects include erectile dysfunction and uncontrollable peeing. But these side effects don’t occur in everyone who has a prostatectomy.
You can’t touch it. But you can feel it from the outside of your body or through your anus.
The easiest way to feel your prostate is from the back half of the area of skin between your anus and genitals, closest to your anus. The area mainly contains nerves and veins, not tissue. Your prostate should feel round and soft or rubbery, like the tip of your nose.
You can also feel your prostate more directly through your anus. It’s about 2 inches inside (about two knuckles in on your finger). Gently curl your finger upward, toward your body. It should feel round and soft or rubbery.
Advertisement
When you touch your prostate, either through your perineum or your anus, you may feel a sudden urge to pee.
Many find that prostate massage feels sexually satisfying. But you can’t accurately check your prostate health through a self-exam. If you have concerns about your prostate, talk to your healthcare provider. They can answer any of your questions and accurately check your prostate health.
Your prostate’s main purpose is to create fluids in your semen and force semen through your urethra when you ejaculate. Your prostate will likely get larger as you age, which is normal. But prostate cancer is the second most common cancer that affects males. It’s a good idea to get regular prostate cancer screenings after you turn 50. Changes to your peeing habits, blood in your pee or semen, pain in the area or problems getting or keeping an erection may point to problems with your prostate. If you notice any changes, reach out to a healthcare provider.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have a condition that’s affecting your urinary system, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
